Abstract
Background: Murine models of myelodysplastic syndromes (MDS) exhibit lower bone mass (B-Mass), and several reports suggest increased incidence of osteoporosis and fractures in MDS patients. Whether MDS is associated with lower B-Mass is unknown.
Aims: 1) to develop a simple method to estimate trabecular B-Mass from bone marrow biopsies (BMB); 2) to compare the trabecular B-Mass of MDS patients at diagnosis and non-MDS controls; 3) to develop an artificial intelligence (AI) algorithm for automated trabecular B-Mass assessment.
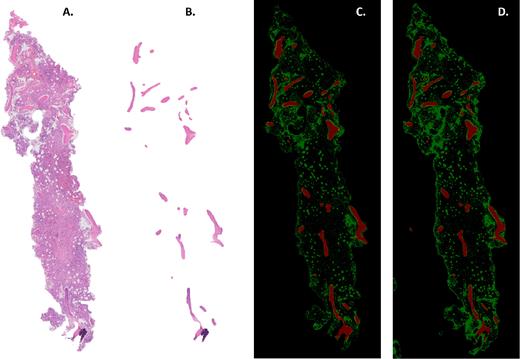
Methods: In this study we included male patients age ≥ 65 years old with "lower-risk" (LR) MDS, diagnosed at Tel Aviv Sourasky Medical Center, between 2011 and 2019 and age-matched controls undergoing bone marrow (BM) biopsy for either unexplained anemia or as a part of staging work-up for newly diagnosed lymphoma. BM slides (H&E stain) were digitally scanned. The total relevant area (TRA, Figure 1A) was identified and bone trabeculae were manually contoured using Adobe Photoshop software. Bone area (BA, figure 1B) was calculated as the sum of all contoured pixels of bone, and B-Mass = BA/TRA(%). The manually annotated data were used to develop a preliminary AI algorithm to automatically detect the BA as well as BM fat for use in the current and future research in the field. The Sørensen-Dice similarity coefficient (DSC) was used to assess agreement between manual and AI annotations.
Results: There were 43 MDS and 36 control patients with mean ages of 80 and 78 years (p>0.05), respectively. Comorbidities in both groups were similar. Notably, trabecular B-Mass of MDS was significantly lower than that of controls: 11.6% [95%CI 9.9-13.3] vs 18.3% [16.6-20.3], respectively (p<0.0001). This represented a 37% relative reduction for MDS patients compared to controls. Next, the manually annotated data used to develop an AI algorithm automatically assessed trabecular B-Mass. The devised algorithm, tested on 17 patient samples, yielded a DSC (Mean ± SEM) of 0.76 ± 0.015 and 0.81 ± 0.02 for bone and fat respectively (Figure 1C and 1D).
Conclusions: We have developed a simple technique to estimate trabecular B-Mass based on available BM sections. Importantly, we found that trabecular B-Mass of LR-MDS patients is compromised already at diagnosis. In addition, automated (AI) assessment of B-Mass using available H&E-stained BM slides is feasible and clinically relevant for patients with MDS and other hematological malignancies. Future work will develop the AI technique and expand it to identify all components of the BM, including the cellular compartment. This will enhance our understanding of the osteohematological niche in such patients, and aid in diagnosis as well as treatment planning.
This study was supported by a grant from the Dotan Hemato-oncology Fund, the Cancer Biology Research Center, Tel Aviv University to DN, MM and HSO.
Figure 1: Bone marrow biopsy (BMB) slide of a representative patient showing (A) the total relevant area, and (B) the bone area - TRA and BA respectively. Demonstrating the artificial intelligence (AI) technique for the same patient, we compare (C) manual annotation to (D) AI-based annotation of both bone (red) and fat (green).
Mittelman: Janssen · Roche · Novartis · Takeda · Medison / Amgen · Neopharm / Celgene / BMS · Abbvie · Gilead: Research Funding; Novartis · Takeda · Fibrogen · Celgene / BMS · Onconova · Geron: Other: Clini; Onconova · Novartis · Takeda · Silence: Membership on an entity's Board of Directors or advisory committees; MDS HUB: Consultancy; Celgene / BMS · Novartis: Speakers Bureau.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal